Alcohol Liver Disease
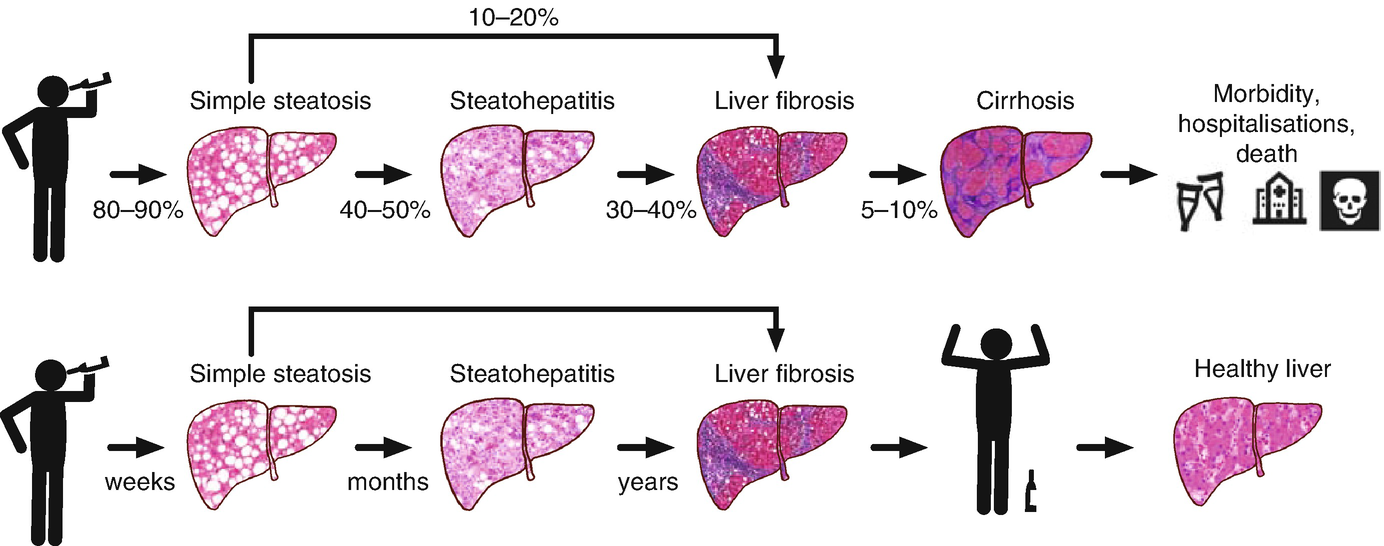
Alcoholic liver disease is a spectrum of disease which is manifested due to over consumption of alcohol. It is of following types:
- Fatty liver
- Alcoholic hepatitis
- Cirrhosis
Alcoholic liver disease is one of the most common diseases prevalent in Nepal. Its incidence is increasing day by day in Nepal as well as whole world.
Risk factors:
- Quantity of alcohol intake: In men, 40-80 g/ day of alcohol ingestion produces fatty liver.160 g/ day for 10- 20 years causes hepatitis or cirrhosis. Only 15% of alcoholics develop alcoholic liver disease.
- Gender: Women are more prone to develop alcoholic liver disease. Amount greater than 20 g/day produces alcoholic liver disease in women.
- Hepatitis C infection: Concomitant infection with hepatitis C in patients with alcoholic liver disease increases the severity even at a younger age.
- Genetics: Patatin like phospholipase domain containing protein 3 has been associated with alcoholic cirrhosis.
- Metabolic disorders: Disorders such as haemochromatosis, Wilson's disease are at high risk of developing alcoholic liver disease.
- Malnourishment
Pathophysiology:
The exact mechanism behind alcoholic liver disease is unknown. It is most likely due to release of pro-inflammatory cytokines (TNF- Alpha, IL-6 and IL-8), acetaldehyde toxicity and oxidative stress. These pro- inflammatory cytokines cause inflammation, apoptosis and later fibrosis.
Alcoholic fatty liver:
It is due to accumulation of fatty acids in the hepatocytes. It is a reversible condition. Alcohol abstinence can revert fatty liver within 3 months.
Alcoholic hepatitis:
It occurs due to release of pro-inflammatory cytokines which leads to inflammation of hepatocytes. The inflammatory cytokines responsible for hepatitis are TNF-alpha, IL-6 and IL-8. These cytokines cause apoptosis and necrosis of liver cells. It is a reversible condition. Alcohol abstinence can reverse the condition within 6 months.
Cirrhosis:
Cirrhosis is defined as a chronic liver condition characterized by
- Loss of hepatocytes
- Formation of fibrosis
- Formation of regenerative nodules
- Loss of normal architecture of liver
These changes lead to decrease in hepatocellular mass and an alteration in blood flow. Fibrosis occurs with activation of hepatic satellite cells resulting in increased amount of collagen formation and other components of extracellular matrix.15-20 % of heavy drinkers develop cirrhosis.
Clinical features:
- Fatty liver:
Patients are mostly asymptomatic. Patient may present with lethargy, anorexia, nausea, vomiting, pain abdomen.
- Alcoholic hepatitis:
Most of the patients are asymptomatic. Patients may present with pain abdomen, nausea, vomiting, lethargy, jaundice, hepatomegaly. Portal hypertension, ascites or variceal bleeding can occur in the absence of cirrhosis.
- Cirrhosis:
Patients can present with non specific symptoms such as abdominal pain, fever, nausea, vomiting, diarrhoea, anorexia and malaise. Patients may present with specific complications of chronic liver disease such as ascites, oedema and upper gastrointestinal bleeding. Other clinical manifestation includes jaundice or encephalopathy. Physical examination reveals enlarged liver and spleen with liver edge being firm and nodular. Other frequent findings include palmar erythema, spider naevi, parotid gland enlargement, digital clubbing, muscle wasting. Men have decreased body hair, gynaecomastia and testicular atrophy. In women, menstrual irregularities occur and some women may be amenorrheic.
Diagnosis:
Lab findings:
- Fatty liver: Mostly normal. There may be mild elevation in liver enzymes (ALT,AST), bilirubin.
- Alcoholic hepatitis: the ratio of AST: ALT is >2:1.AST and ALT are usually elevated two to seven fold. They are rarely >400 IU.AST: ALT ratio is due to deficiency of pyridoxal phosphate. Another reason is due to alcohol mediated hepatic mitochondrial injury releasing more AST. Other findings include increase in gamma glutamyl transferase,alkaline phosphatase and bilirubin.
- Cirrhosis: There is elevation in liver enzymes (AST.ALT). There is rise in bilirubin. The synthetic function of the liver is lost with hypoalbuminemia and increased prothrombin time.
Imaging:
Ultrasonography: Ultrasonography of the abdomen reveals fatty liver in case of alcoholic fatty liver. In alcoholic hepatitis there is hepatomegaly. In cirrhosis there are features of portal hypertension such as ascites, splenomegaly and increase in portal vein diameter.
Liver biopsy:
The hallmark of alcoholic hepatitis is hepatocyte injury characterized by ballooning degeneration,spotty necrosis, polymorphonuclear infiltrate and fibrosis in the perivenular and perisinusoidal space of Disse. Mallory -Denk bodies can also be present in florid cases but are not specific. Liver biopsy in cirrhosis can be done to rule out other causes of cirrhosis (Viral hepatitis, Autoimmune hepatitis).
Treatment:
- Alcohol abstinence is the cornerstone of treatment.
- Corticosteroids or pentoxifylline can be used in alcoholic hepatitis after calculating Discriminant function or Model for End Stage Liver Disease score. Discriminant function ≥32 or MELD score ≥ 21 requires treatment with prednisolone.
- Liver transplantation is reserved for cases with advanced liver disease.
- Adequate nutritional support should be provided to patients with alcoholic liver disease.
Prognosis:
Critically ill patients with alcoholic hepatitis have short term (30 day) mortality rates > 50 %.Discriminant function score ≥ 32 and Model for End Stage Liver Disease ≥ 21 is associated with significant mortality in alcoholic hepatitis. In a patient who develops complications of cirrhosis and who continues to drink, 5 year survival is < 50%.


